The Role of Hormones in Each Phase of the Menstrual Cycle
The Role of Hormones in each phase of the Menstrual Cycle is a complex interplay of hormones that prepare the female body for pregnancy each month. Understanding the role of these hormones can provide insights into reproductive health, the causes of menstrual irregularities, and the impact of hormonal fluctuations on overall well-being. This blog will delve into the hormonal changes that occur during each phase of the menstrual cycle, explaining their functions and significance.
Overview of the Menstrual Cycle
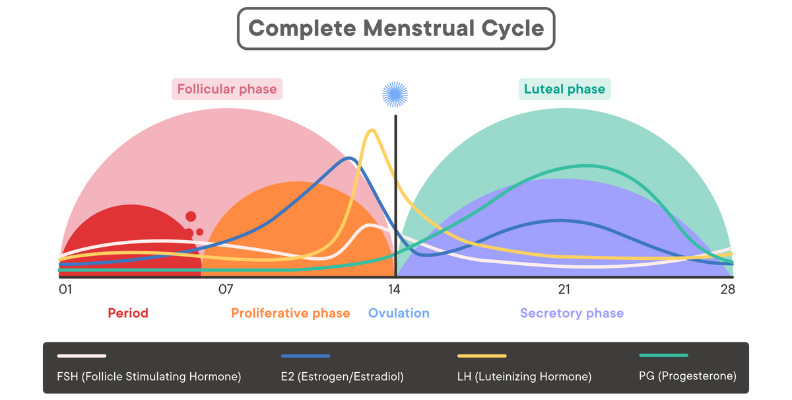
The menstrual cycle typically lasts about 28 days, but it can range from 21 to 35 days in adults. It is divided into four main phases:
- Menstrual Phase
- Follicular Phase
- Ovulation Phase
- Luteal Phase
Each phase is driven by hormonal changes orchestrated by the hypothalamus, pituitary gland, and ovaries. The primary hormones involved are estrogen, progesterone, follicle-stimulating hormone (FSH), and luteinizing hormone (LH).
1. Menstrual Phase
What Happens During the Menstrual Phase?
The menstrual phase marks the beginning of the menstrual cycle and typically lasts 3-7 days. During this phase, the endometrial lining, which thickened in preparation for a potential pregnancy, is shed if fertilization has not occurred. This results in menstrual bleeding.
Hormonal Changes
- Decline in Estrogen and Progesterone: At the end of the previous cycle, the levels of estrogen and progesterone drop sharply. This decrease triggers the shedding of the uterine lining.
- FSH Levels Begin to Rise: As estrogen and progesterone levels fall, the pituitary gland increases the production of FSH. This hormone stimulates the growth of ovarian follicles for the next cycle.
Significance
The menstrual phase clears the old endometrial lining, making way for the new cycle. The rise in FSH marks the transition to the follicular phase, initiating the development of new ovarian follicles.
2. Follicular Phase
What Happens During the Follicular Phase?
The follicular phase overlaps with the menstrual phase and continues until ovulation, typically lasting from day 1 to day 14 of the cycle. During this phase, the ovarian follicles mature, and the uterine lining starts to rebuild.
Hormonal Changes
- FSH and Follicle Growth: Rising levels of FSH stimulate several ovarian follicles to grow. Each follicle contains an egg, but usually, only one follicle becomes dominant and continues to mature.
- Increase in Estrogen: As the follicles grow, they produce increasing amounts of estrogen. Estrogen has several roles:
- Uterine Lining Regrowth: Estrogen stimulates the thickening of the endometrial lining.
- FSH Regulation: High levels of estrogen eventually inhibit further FSH production, preventing multiple follicles from maturing fully.
- Low LH Levels: Initially, LH levels remain low, but they gradually increase as the follicular phase progresses.
Significance
The follicular phase prepares the ovaries to release a mature egg and rebuilds the uterine lining, creating an optimal environment for potential implantation.
3. Ovulation Phase
What Happens During the Ovulation Phase?
Ovulation is the release of a mature egg from the dominant ovarian follicle, typically occurring around day 14 of the cycle. The egg then travels down the fallopian tube, where it may be fertilized by sperm.
Hormonal Changes
- LH Surge: A significant increase in estrogen levels leads to a surge in LH, known as the “LH surge.” This surge is crucial for triggering ovulation.
- Release of the Egg: The LH surge causes the mature follicle to rupture and release the egg.
- Increase in Basal Body Temperature: Progesterone, produced by the ruptured follicle, causes a slight increase in basal body temperature, which can be used to identify ovulation.
Significance
Ovulation is the key event of the menstrual cycle, providing the opportunity for fertilization and pregnancy. The LH surge and subsequent ovulation mark the transition from the follicular phase to the luteal phase.
4. Luteal Phase
What Happens During the Luteal Phase?
The luteal phase follows ovulation and lasts approximately 14 days, ending with the start of the next menstrual cycle. During this phase, the body prepares for a potential pregnancy.
Hormonal Changes
- Corpus Luteum Formation: After releasing the egg, the ruptured follicle transforms into the corpus luteum, which secretes progesterone and some estrogen.
- Rise in Progesterone: Progesterone levels increase significantly, supporting the thickening of the endometrial lining and making it receptive to a fertilized egg.
- Moderate Estrogen Levels: Estrogen levels remain elevated but are secondary to progesterone during this phase.
- FSH and LH Decline: Elevated progesterone and estrogen inhibit the production of FSH and LH, preventing the maturation of new follicles.
If Fertilization Occurs
- hCG Production: If fertilization and implantation occur, the developing placenta produces human chorionic gonadotropin (hCG). This hormone maintains the corpus luteum and its production of progesterone.
- Continued Progesterone Production: The sustained levels of progesterone prevent the shedding of the endometrial lining, supporting the early stages of pregnancy.
If Fertilization Does Not Occur
- Corpus Luteum Regression: In the absence of hCG, the corpus luteum degenerates after about 10-12 days.
- Decline in Progesterone and Estrogen: The regression of the corpus luteum leads to a drop in progesterone and estrogen levels.
- Onset of Menstruation: The decrease in these hormones triggers the shedding of the endometrial lining, marking the beginning of a new menstrual cycle.
Significance
The luteal phase is critical for maintaining the endometrial lining and supporting early pregnancy if fertilization occurs. If pregnancy does not occur, the decline in progesterone and estrogen prepares the body for menstruation.
Conclusion
The menstrual cycle is a finely tuned process regulated by the intricate interplay of hormones. Each phase—menstrual, follicular, ovulation, and luteal—depends on the precise timing and balance of these hormones to ensure reproductive health and the potential for pregnancy. Understanding these hormonal changes can provide valuable insights into managing menstrual health, addressing irregularities, and enhancing overall well-being.
Key Points to Remember
- Estrogen: Dominant during the follicular phase, responsible for thickening the endometrial lining and regulating FSH.
- Progesterone: Dominant during the luteal phase, crucial for maintaining the endometrial lining and supporting early pregnancy.
- FSH: Stimulates follicle growth in the ovaries.
- LH: Triggers ovulation and the formation of the corpus luteum.
By recognizing the roles of these hormones, individuals can better understand The Role of Hormones in each phase of the Menstrual Cycle and seek appropriate care when needed. Whether dealing with menstrual irregularities, planning for pregnancy, or managing reproductive health, knowledge of the menstrual cycle’s hormonal dynamics is empowering and essential for making informed health decisions.